Mountain Comprehensive Health Corporation fortifies their rural health program, adding significant value for their patients using the 340B Program.
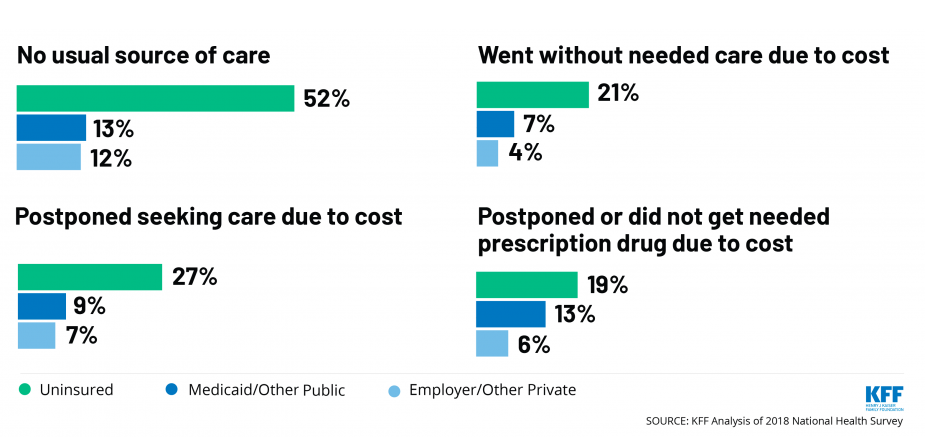
The uninsured are some of the most vulnerable patients, even more so than those on Medicaid or with private insurance.
The low-income and uninsured are most likely to:
- Go without care
- Postpone care due to cost
- Have poor health outcomes
- Postpone a needed prescription drug due to cost
What are the benefits of implementing a program to provide access to affordable prescription medications for your uninsured patients?
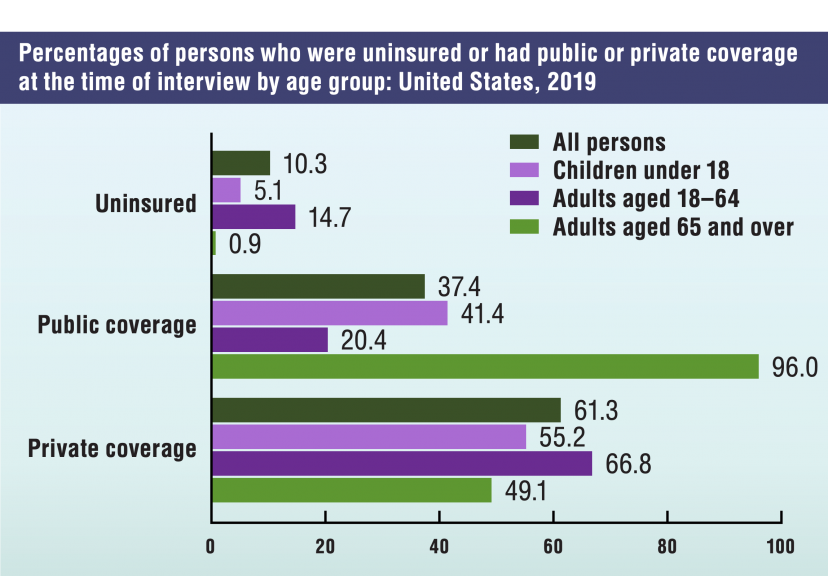
Uninsured patients can represent a significant patient base for virtually every hospital, Community Health Center and FQHC. Providing your uninsured patients with access to affordable prescription drugs provide:
- A welcome relief for individuals to be able to afford their prescriptions
- Decreased risk of future uncompensated care and the potential for hospital admissions
- Better healthcare outcomes, due to adherence
- Improved community perceived support and increased patient satisfaction


This exclusive Mystery Box Experience features a fun group appetizer competition.
DATE: Tuesday, March 28, 2023, from 6:30PM – 9:30PM
LOCATION: San Diego Wine and Culinary Center
EVENT: SUNRx Exclusive Mystery Box Experience
Sign up below!
What’s the Mystery Box Appetizer Competition?
In this exciting competition, a Mystery Box of ingredients will await each team at their cooking station.
A box will be provided for each team of 4-6 participants.
Each team will open their box to reveal a variety of ingredients
The ingredients will be used to create a signature appetizer item using your creativity!
Experience Schedule
Reception @ 6:30 PM
After arriving to the location, we will check you in. Allow yourself some time to enjoy cocktails before the Experience.
Experience @ 7:00 PM
Mystery Box Appetizer Competition
Dinner @ 8:00PM – 9:30PM
Dinner, drinks, and dessert will be served following the Mystery Box Appetizer Experience.

July 10-12, 2023
Washington, DC | National Harbor, MD
Schedule a meeting below!
ThoughtSpot 2023
 GO TO EVENT SITE
August
GO TO EVENT SITE
August



